Know the Full Cost of Fast and Cheap
You hired the archiving vendor with the lowest price and shortest timeline, but three weeks from going live and a month from decommissioning your legacy systems, something is terribly wrong: the archive seems to be missing data and images. An extra 90 days has just been added to your timetable, and that means you’ll have to pay to keep your legacy systems running. You also need the resources to fix problems that arise during that extended period as well as continue dedicating staff to maintain multiple systems. Archiving legacy systems and the options that accompany the process can appear simple at first glance. However, many unplanned and unbudgeted complexities often arise mid-project.
Regardless of the speedbumps some hospitals and health systems face along their data archiving journey, archiving solutions continue to be in high demand. Yet, health systems sometimes experience buyer’s remorse. This can happen when decisions are made under budgetary and time pressures, when there are misconceptions about the process and priorities, or when strategies are short-term. Cost-cutting is a necessary goal for hospitals and health systems, particularly when inflation creates rising equipment costs and the fight for talent increases due to fallout from COVID-19. Short-term resource management cannot be the only consideration, especially if it will cost both time and money in the end. However, there are ways to avoid that.
On the surface, the archiving process involves three main steps:

DATA EXTRACTION

DATA CONVERSION

DATA ARCHIVING
But what happens in between is complex and unique to the current and future needs of the specific hospital or health system.
“There is no ‘one-size-fits-all’ when it comes to archiving, but there are a number of best practices to model and pitfalls to avoid. The right archiving strategy results in access to the data you need for every stakeholder, when and how you need it, now and in the long run.”
Jim Jacobs | MediQuant President and CEO.
What Does Successful Archiving Look Like? And How Can Health Organizations Achieve it?
From the moment a new electronic health record (EHR) system is selected the data archiving journey begins. Insight gleaned from years of data archiving experience and dozens of client stories suggest a data archiving journey that breaks down into several decisions, each of which have opportunities to work seamlessly and improve the necessary data access or not work at all. The financial consequences of the wrong choices are tangible.
Start the Planning Process Early, Set Long-Term Goals
Underestimating the size and complexity of the task is a frequent problem. According to MediQuant Chief Clinical Officer & Vice President, Government Strategy, Kel Pults, DHA, MSN, RN-BC, NREMT, “Many health system transformations are planned with an assumption that transferring data is as simple as loading a truck with file boxes, driving it to a new location and setting it down.”
The College of Healthcare Information Management Executives (CHIME) believes the issue is one of prioritization. “New HIS implementations overshadow data management and data archiving programs, strapping both IT resources and budgets, and pushing initiatives to manage legacy system data to the back burner.”
MediQuant Vice President, Solution Delivery, Shelly Disser, DBA., suggests preferably starting the archiving project along with the EHR transition by setting definite goals and a distinct plan with a tentative go-live date.
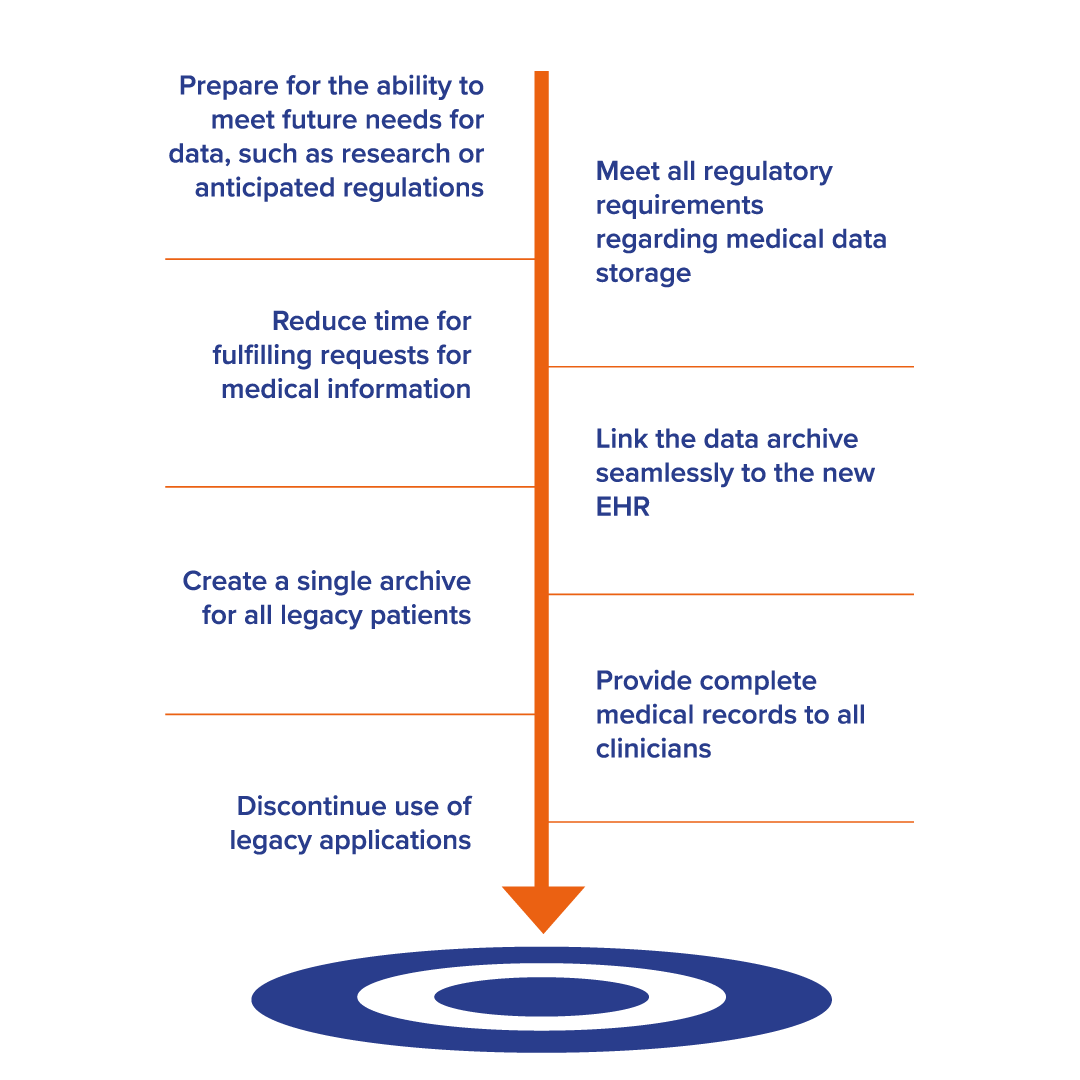
Examples of project goals include:
Establish a Budget That Matches the Goals
The budget and goals should account for what each stakeholder needs to do with the data today and in the future. For example, non-discrete data archiving – involving file types such as PDFs and images – is less expensive but has critical limitations. By comparison, discrete data helps with use cases across teams and has the flexibility to allow for future demands. It can ensure success with things like HIM requests and complete compliance with Information Blocking.
The wrong archival procedure to meet these needs often leads organizations to revamp and revise later. Beware automated archiving methods that extract data in one large PDF. These are indeed fast and cheap, but do not make crucial information either searchable or useable. Similarly, importing data into systems like Microsoft’s OnBase for documents and processes will only increase efficiency if the data is organized by use case for different stakeholders.
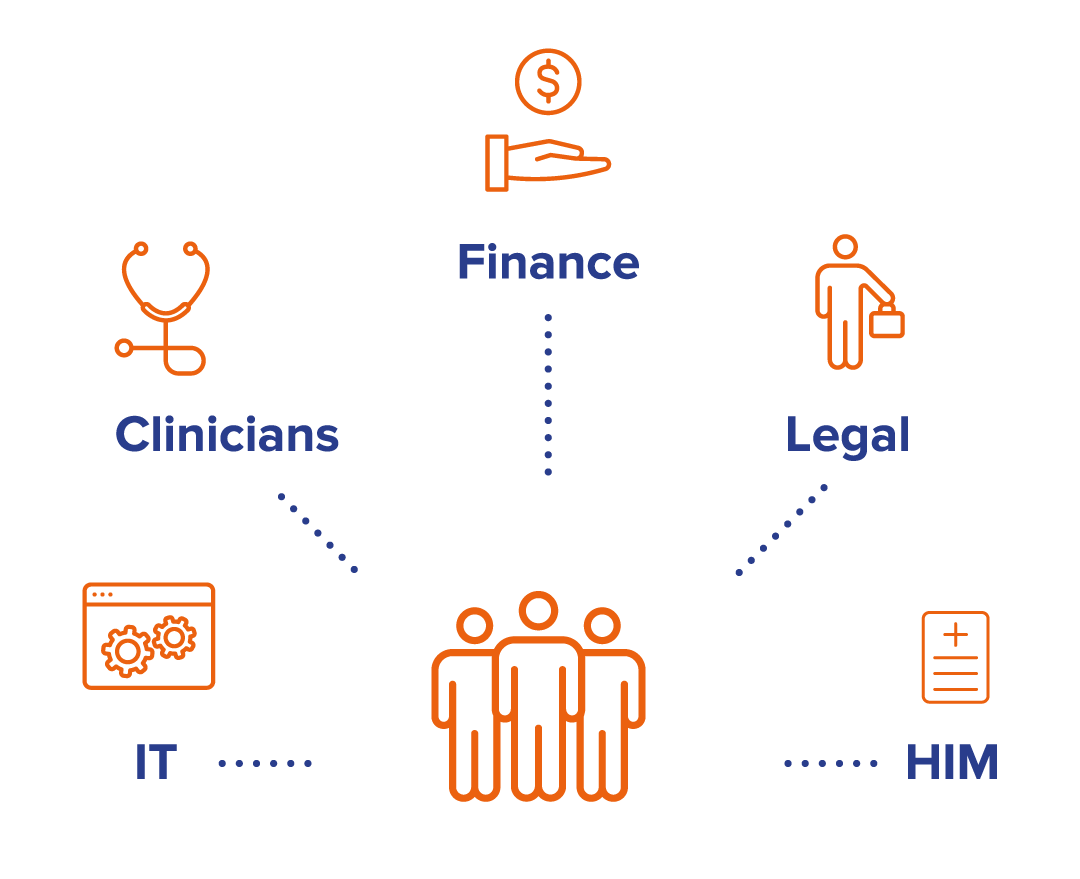
Create an Archiving Project Team
Dave Lamar, MediQuant’s Chief Growth Officer notes that “it’s commonly accepted to assign a team of resources to support a new EHR system installation. Taking systems offline may require a similar effort.”
Planning early helps to enlist the right mix of stakeholders on the archiving project team. One IT Operations manager noted that SMEs are important in helping to understand workflow, nuances, etc., and can help with data validation. He strongly suggested “using subject matter experts before they train on the new system and forget the old.”
The most effective teams involve the appropriate clinicians (doctors, nurses, pharmacists, lab technicians) and/or finance staff, in addition to IT, HIM and legal staff. They assign project oversight and who will work on different aspects such as data entry and database management – considering the team’s other duties that might cause undue disruptions to either the project or their workflow. Depending on the situation and staffing, it may be best to contract external workers. Both internal commitments and external resources should be considered in the budgeting process.
Choose the Right Archiving Partner
The variety of available archiving vendors keeps growing, many focused on making the process cheap, quick and easy. That may be appropriate in some cases, but archiving is complicated and nuanced. Frequent concerns arise around data quality, accessibility, and lack of useability if checks and balances with multiple data validations are ignored, and if there are no contingency plans to manage potential mistakes, hold-ups and surprises. Each challenge can delay the go-live date, which means keeping legacy systems running longer, and all the associated expenses.
An experienced archiving partner that has handled numerous projects can help the client avoid errors, wasted time, lost confidence, extra tests, bad ROI reports and legal issues. A worthy partner with intellectual property acquired and honed over years will anticipate issues with extraction and migration of specific systems and different types of clinical, financial and enterprise resource planning data. The right partner can also provide counsel to help health systems manage projects at scale and support an enterprise-wide archiving strategy.
Sound expensive? Consider the cost faced by facilities when they need to hire a new vendor to fix mistakes or start from scratch, both of which result in additional expenditure of time and money. Even worse, mistakes and misunderstandings can lead to issues with data quality and accessibility.
Valued archiving partners can help ward off these issues by offering the resources and project management to handle it all:
- A clear initial, agreed-upon scope of work and expectations that matches your goals, including realistic timelines and allowances for issues along the way
- Recommendations and stewardship services to help with planning
- Consultants with strong clinical, financial, enterprise and implementation backgrounds
- Discovery to confirm the data in the legacy system
- An experienced technical team to extract the data
- Data modelers to migrate the data into the archiving solution
- A data validation process to ensure it is complete, accurate, clean and uncompromised
- Experience with diverse EHRs, especially the most complicated
- Proven, reliable technology with modules and interfaces that keep data accessible
- The breadth of services, solutions and methodologies to handle the entire journey
Determine What Data to Archive
Knowing what and how to store clinical information has always been a challenge for hospitals and health systems. There are so many things to consider, including the volume of data, the number of legacy systems, short- and long-term needs, compliance, data governance policies, security, and costs.
Dr. Pults notes, “When you treat a patient, you want to have every bit of available data there to help you.” The decision process boils down to archiving the legacy applications that are no longer needed while keeping the data that is, by making it easy to work with. Decide what data to keep in an active archive, what to move to a static archive, and what to destroy. Create an inventory of all legacy systems, noting which type of data is managed — clinical, patient accounting or both. List the uses and potential need to access data, potentially frequently, within another workflow. Ensure that any HIM request can be answered while complying with information blocking.
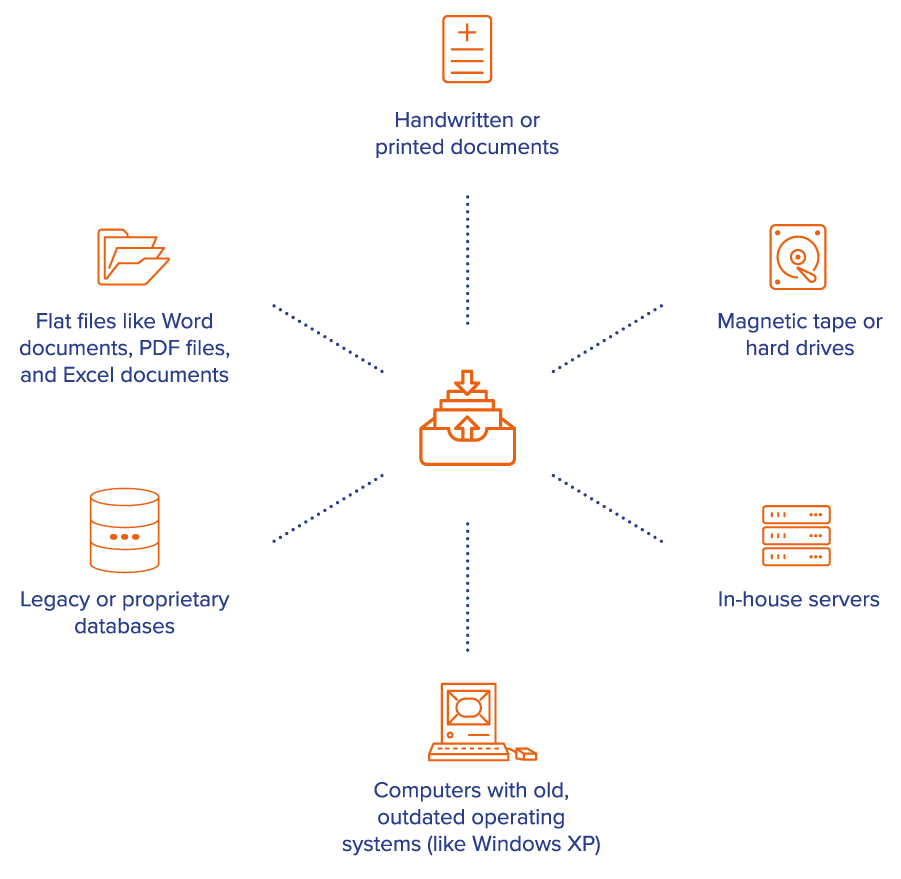
The right archiving partner knows what to look for, where to look for it and how to pull it out. Some hospital systems may be tempted to handle this process internally – whether due to cost or fear of data loss. But most health systems are less adept at the process than a qualified outside service. The right service can help avoid the cost and delays of inefficient DIY extraction and will have extraction experience with a wide range of EHR brands, both major market holders and proprietary ones; multiple databases; different healthcare areas; and different varieties of data that can be trapped in your EHR, such as faxes, scans, or media attachments.
Decide How to Transform Data
Choosing the User Experience and Saving Long-Term Cost
To convert data into a form or structure that meets the new system’s requirements, several critical decisions must be made: whether and what to convert to discrete or structured records in a database versus creating non-discrete data or static images.
While there is a place for both non-discrete and discrete data, a static archive consisting only of a single gigantic PDF is unusable. It may be inexpensive, but it won’t serve anyone well. Non-discrete data can’t be easily pulled into reports or used for analytics – something that might be needed in the future. A clinician who needs a specific lab report might need to scan through a 100-page PDF to find it. Instead of accessing only the relevant data needed to fulfill release of information (ROI) requests, entire reports and documents must be released, making this archiving approach less than ideal for litigation cases. That could be a costly mistake. Conversely, discrete data is collected and stored in a database table with an important level of detail. This type of data is accessible, measurable and reportable.
An active archive preserves data in an accessible and actionable format that transforms it into a muti-faceted asset. This type of solution promotes interoperability, optimizes clinical care, facilitates data for legal and compliance purposes, and enables AR work-downs and revenue retrieval.
An active archive solution further promotes cost savings by eliminating extraneous outside system management vendor fees and reducing staff resources used to maintain legacy systems. Our customers have experienced as much as an 80 percent reduction in expenses. One IT operations manager noted the ultimate savings of data transformation decisions: A positive cost-benefit ratio for every project and every step based on both the savings from decommissioning legacy systems and emerging AR work-downs with DataArk.
Qualify Each Decision as a Cost-Effective Step Toward Confidence and Trust
For hospital and health system executives entrusted with safeguarding one of their organization’s most valuable assets, an extensive assessment of the long-term ramifications and advantages of data archiving is paramount. While it’s acknowledged that most data managers do not engage in archiving transformations on a daily basis, those who carefully weigh each decision and rely on the expert guidance of an experienced archiving partner can gain confidence in the process and the potential return on investment. Collaboration and the alignment of collective objectives among stakeholders will result in optimized patient care while meeting compliance, legal and research needs – now and in the future.


